The uvea is a vascular stratum that includes the iris, ciliary body and choroid. Uveitis is defined as inflammation of a part of the uvea or its entirety, but it is also used to describe inflammatory processes of any part of the eye, such as the vitreous or peripheral retina. The clinical taxonomy of uveitis is contingent upon the affected anatomy. Anterior uveitis, also known as iridocyclitis, is characterized by inflammation of the iris and ciliary body. Intermediate uveitis is inflammation of the vitreous or peripheral retina; it also includes pars planitis, posterior cyclitis and hyalitis. Posterior uveitis affects the retina and choroid. Panuveitis affects the entire uveal tract. Consisting of 25+ different disease characteristics, uveitides ranks fifth in the leading causes of blindness in the USA.1 Uveitis, along with its secondary complications and adverse effects from long-term treatment, is estimated to be the cause of 5–20% of cases of blindness in developed countries and 3–10% of such cases worldwide.2,3 Noninfectious uveitis (NIU), as implied by its name, arises from an underlying inflammatory or autoimmune mechanism rather than from an infectious one. Anterior uveitis is the most common manifestation of uveitis, accounting for an estimated four in five cases of all NIU.4 The estimated incidence of best-corrected visual acuity (BCVA) becoming 20/400 or worse in patients affected by anterior uveitis is 2.41 per 1,000 person-years.5 In the USA, the estimated prevalence of NIU stands at approximately 121 per 100,000, accounting for approximately 91% of all cases of uveitis.4,6 The demographically most at-risk population in developing NIU is the working-age group, with ages 20–50 years. Within this age group, being non-Hispanic white, female sex and having concurrent autoimmune disease are also demographical risk factors.7 In the USA, the prevalence of the specific types of uveitis varies among different ethnic groups. Black individuals are more commonly affected by anterior uveitis, Hispanics by intermediate uveitis and white non-Hispanics by posterior uveitis.8 Lifestyle risk factors include smoking and vitamin D deficiency. Conditions predisposing to uveitis span a spectrum of autoimmune disorders (juvenile idiopathic arthritis [JIA], ankylosing spondylitis, psoriatic arthritis, Kawasaki disease, inflammatory bowel disease, connective tissue disorders and many more, as given in Table 1), trauma, cancers and adverse effects of medication. The HLA-B27-associated diseases are highly associated with acute unilateral NIU and are the leading known cause of acute anterior uveitis (AAU) in developed countries, with a 2.5:1 male-to-female predominance ratio.9
Table 1: Autoimmune aetiologies of noninfectious uveitis: Clinical presentation, uveitis type, laboratory findings and treatment
|
Condition |
Symptoms/findings |
Typical uveitis type |
Associated laboratory/imaging findings |
|
Behçet’s disease |
Oral ulcers, genital ulcers and skin lesions |
Anterior, posterior and panuveitis |
No specific serum findings |
|
HLA-B27-associated uveitis |
Acute anterior uveitis and asymmetric oligoarthritis |
Anterior uveitis |
Positive serum HLA-B27 |
|
Sarcoidosis |
Granulomatous inflammation, cough and dyspnoea |
Anterior and posterior uveitis |
Elevated serum ACE, hypercalcaemia, positive serum HLA-DRB1, bilateral hilar adenopathy and reticular opacities on chest X-ray |
|
Juvenile idiopathic arthritis |
Joint pain/swelling, morning stiffness and antalgic gait |
Anterior uveitis |
Can be seronegative or seropositive for ANA, RF and CCP—highest risk for uveitis in those who are seropositive |
|
Vasculitides |
Rash, joint pain and fever |
Intermediate and posterior uveitis |
Marked elevation in ESR/CRP, stenosis, occlusion or aneurysmal dilation of affected blood vessels on CT |
|
Multiple sclerosis |
Vision loss, weakness and numbness |
Intermediate uveitis |
Oligoclonal bands, pleocytosis on CSF and hyperintense periventricular lesions on MRI |
|
Vogt–Koyanagi–Harada disease |
Headache, tinnitus, alopecia and vitiligo |
Panuveitis |
Pleocytosis on CSF, delayed choroidal perfusion, peripapillary hypercyanescence and leakage on ICGA |
|
Kawasaki disease |
Fever, rash, conjunctivitis and coronary aneurysms |
Anterior uveitis |
Elevated ESR/CRP, anaemia, leucocytosis, thrombocytosis, albuminaemia, elevated ALT and pyuria |
|
Blau syndrome |
Arthritis, rash and uveitis |
Panuveitis |
No specific serum findings; noncaseating granulomas on skin biopsy and NOD2 gene mutation on next-generation sequencing |
|
Tubulointerstitial nephritis and uveitis syndrome |
Renal symptoms, fever and rash |
Anterior uveitis |
Elevated serum BUN, creatinine and B2M; proteinuria and pyuria on UA and cortical hyperechogenicity on renal US |
|
Relapsing polychondritis |
Auricular/nasal/tracheal chondritis, arthritis and respiratory symptoms |
Anterior uveitis |
No specific serum findings; airway trapping, narrowing and collapse on CT |
|
Sjögren’s syndrome |
Dry eyes, dry mouth and parotitis |
Anterior and posterior uveitis |
Positive serum anti-SSA and anti-SSB |
|
Crohn’s disease |
Abdominal pain, diarrhoea and weight loss |
Anterior uveitis |
Elevated serum CRP, ESR and ASCA; normal serum ANCA; elevated calprotectin in stool analysis and colonic abscesses and fistulas on MRE/CT |
ACE = angiotensin‐converting enzyme;ALT = alanine transaminase;ANA = antinuclear antibody;ANCA = antineutrophilic cytoplasmic antibody;ASCA = anti-Saccharomyces cerevisiae antibodies;B2M = beta-2 microglobulin;BUN = blood urea nitrogen;CCP = cyclic citrullinated peptide;CRP = C-reactive protein;CSF = cerebrospinal fluid;CT = computed tomography;ESR = erythrocyte sedimentation rate;HLA = human leucocyte antigen;ICGA = indocyanine green angiography;MRE = magnetic resonance enterography;MRI = magnetic resonance imaging;NOD = nucleotide-binding oligomerization domain;RF = rheumatoid factor;SSA = Sjögren’s syndrome-related antigen A;SSB = Sjögren’s syndrome-related antigen B;UA = uric acid;US = ultrasound.
This article aims to provide an overview of NIU management, including current and investigative therapies, with a particular focus on ophthalmic routes, as systemic immunosuppression using antimetabolites and biologics falls beyond the scope of this review.
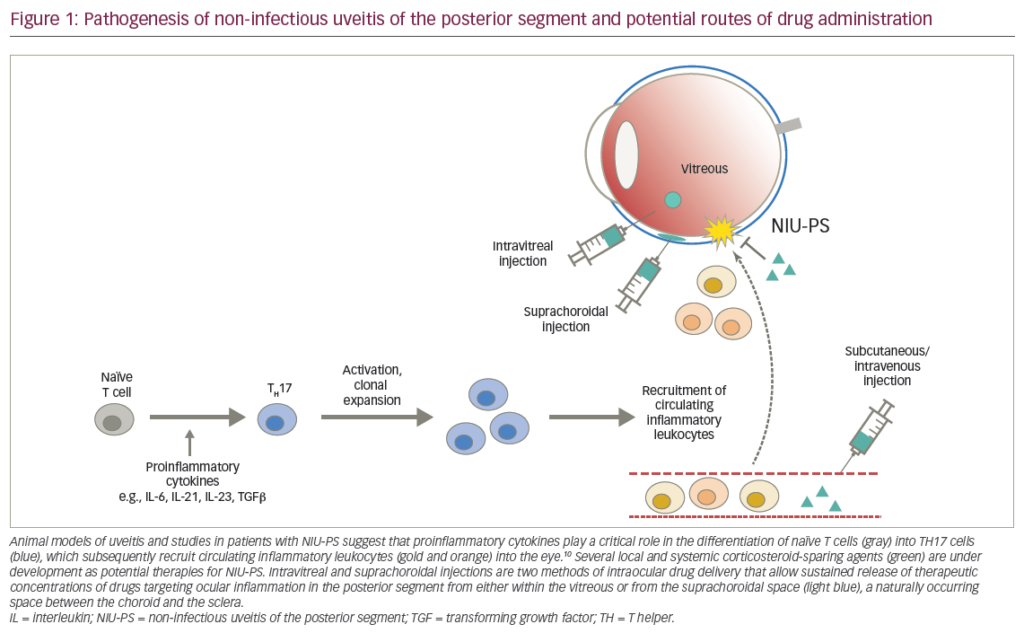
Pathogenesis
Approximately one in three uveitis cases are idiopathic, as observed in the VISUAL I (Efficacy and Safety of Adalimumab in Patients With Active Uveitis) and VISUAL II (Efficacy and Safety of Adalimumab in Subjects With Inactive Uveitis) studies (ClinicalTrials.gov Identifiers: NCT01138657 and NCT01124838).10–12 The majority of cases of chronic anterior uveitis are also idiopathic, estimated at 39–72% annually.13 Although the exact cause of NIU remains multifactorial, aberrant immune insults against ocular tissue and cytokine imbalances play key roles. Immunologically, major histocompatibility complex (MHC) activity, T-cell activation, cytokine release and vascular changes contribute to ocular inflammation. Biochemically, prostaglandins, matrix metalloproteinases and nitric oxide are also implicated. More recently, MHC has been further elucidated through genome-wide association studies to identify genetic risk factors that are associated with ocular inflammation. Genetic studies have also highlighted the prominence of the interleukin (IL)-23R region, which is present in noninfectious uveitides associated with Behçet’s disease, ocular sarcoidosis, Vogt–Koyanagi–Harada disease and AAU.14 NIU, often arising as a complication of systemic conditions and ocular trauma, also highlights the impact of the uvea’s extensive vascularization on disease progression.15,16 Vascular changes in posterior uveitis are especially prominent in the retina and choroid, presenting with abnormalities such as nonperfusion, occlusion, neovascularization, aneurysms and telangiectasia.16
Presentation and evaluation
The clinical spectrum of NIU is characterized by a dichotomy in onset: acute, marked by a swift progression; and insidious, characterized by a gradual inception. The cardinal symptoms encompass a constellation of manifestations: ocular hyperaemia, pain, photophobia, blurred vision and vitreous syneresis, colloquially termed ‘floaters’. These symptoms may precipitate abruptly and escalate without expeditious therapeutic intervention, occasionally resulting in significant loss of visual acuity. Specifically in children, insidious uveitis may remain asymptomatic and elude detection, resulting in irreversible sequelae.17–19
The evaluation of NIU is multifaceted, encompassing a detailed history, comprehensive evaluation of clinical findings, imaging modalities, initial laboratory investigations and additional tests depending on findings.
In the evaluation of uveitis, a comprehensive patient history should encompass not only ocular symptoms but also systemic manifestations that may suggest an underlying aetiology. The presence of arthralgia could indicate a rheumatological condition, while febrile episodes may suggest an ongoing infectious process. It is helpful to probe for potential exposure to sexually transmitted diseases or Mycobacterium tuberculosis. The absence of these systemic symptoms is equally informative as it aids in excluding certain differential diagnoses.
Physical examination involves a detailed slit-lamp examination, which provides a thorough assessment of the anterior segment, revealing potential findings such as keratic precipitates, anterior chamber (AC) cells and flare, iris nodules, posterior synechiae and lens changes. The Standardization of Uveitis Nomenclature (SUN) grading system, which grades inflammation from 0 to 4+ based on cell count observed on slit-lamp examination, is used on initial assessments to help tailor treatment.20 Dilated fundus examination is imperative for assessing posterior segment involvement, such as vitreous cells, optic disc oedema and characteristic inflammatory lesions in the retina or choroid. Advanced imaging modalities play a pivotal role in the diagnosis and management of NIU. Optical coherence tomography (OCT) and fundus fluorescein angiography offer high-resolution visualization of the retinal layers, vasculature and inflammatory changes. For anterior uveitis, anterior-segment OCT is emerging as an assessment tool adjunct to slit-lamp findings to better quantify and characterize the presence of inflammation. For uveitis involving posterior structures, OCT angiography is finding utility by delineating vasculature layers and vascular flow as well as vessel density changes that occur during the active and inactive phases of inflammation involving the choriocapillaris.21
Laboratory investigations may not be needed for first-time cases of unilateral anterior uveitis or iritis; however, for bilateral cases, recurrent flares despite initial treatment or uveitis involving nonanterior structures, laboratory tests become essential for identifying underlying systemic conditions.22 The initial routine workup encompasses a complete blood count, erythrocyte sedimentation rate, C-reactive protein analysis, treponemal and nontreponemal assays for syphilis and a chest X-ray. QuantiFERON Gold testing should be considered in patients from an endemic area or at high risk of having tuberculosis. These initial tests will assist in ruling out infectious or cancerous aetiologies.
A second round of tests may overlap with the initial tests depending on practice. These should be pursued and tailored to clinical history, presentation, initial test results and differential diagnoses. These tests include syphilis immunoglobulin G, fluorescent treponemal antibody absorption, venereal disease research laboratory test, serum angiotensin‐converting enzyme and lysozyme, Lyme serology and interferon-γ release assay. For anterior uveitis, flow cytometry testing for HLA-B27 can be helpful, especially with symptoms suggestive of spondyloarthropathies.23 HLA-B27 testing should be omitted for intermediate and posterior uveitis. For posterior or panuveitis, Behçet’s disease and sarcoidosis should be suspected. One should also consider investigating parasitic infections (toxoplasmosis or toxocariasis) and viral aetiologies (herpes simplex virus, varicella zoster virus and cytomegalovirus). Infectious aetiology should also be considered for patients who are seronegative with anterior uveitis refractory to steroid treatment. Chest computed tomography should be ordered if previous tests and examinations point to sarcoidosis. Other laboratory parameters, such as rheumatoid factor, antinuclear antibody (ANA) and antineutrophilic cytoplasmic antibody (ANCA), provide little value, as the associated conditions extremely rarely manifest with uveitis. However, the presence of retinal vasculitis without significant chorioretinitis should warrant screening for ANA, ANCA and antiphospholipid antibodies.24
Should the previously mentioned evaluations fail to yield a conclusive diagnosis, the pursuit of advanced examinations tailored to the presence of rarer disease entities may be necessary. Brain magnetic resonance imaging should be considered in cases of intermediate, posterior and panuveitis concurrent with neurological deficits.25 Such aetiologies that warrant brain imaging in these patients include multiple sclerosis, primary central nervous system lymphoma (PCNSL), neurosarcoidosis and neuroinfection.26,27 Systemic sarcoidosis can be uncovered using whole-body gallium scan or positron emission tomography, along with histopathological examinations of bronchial lavage fluid or biopsies from lesions, granulomas or lymph nodes.24 Diagnostic vitrectomy is recommended in cases where intraocular lymphoma, a type of PCNSL, is suspected. The selection of these advanced tests should be contingent upon the anatomical classification of uveitis, clinical or preclinical indicators, pertinent medical histories of patients and the exclusion of more common aetiologies.
Current medical therapies
The goal of treatment is to resolve local inflammation and reduce pain, photophobia and inflammation, which are mainly achieved with corticosteroids (CS). The route of delivery is dependent on the initial location of inflammation and can include topical, oral, periocular, intraocular or intravenous infusion. Oral prednisone is usually initiated at 0.5–1 mg/kg/day, with a subsequent tailored tapering regimen.28 Timely intervention with CS is ideal to prevent potential irreversible damage. For uveitis that continues to be poorly controlled, immunosuppressants, such as tumour necrosis factor-α inhibitors, antimetabolites, calcineurin inhibitors and alkylating agents, should be considered.29,30 Topical CS therapy is especially effective for anterior involvement, but it has limited therapeutic effects if the affected tissues include intermediate and/or posterior structures. In these cases, systemic CS are helpful as an adjunct therapy, but adequate stepwise treatment includes immunosuppressants and/or biological agents, intravitreal implants, periocular steroids and even vitrectomy in extensive disease.
Topical corticosteroids
Topical CS are the first-line intervention for acute unilateral anterior uveitis, with prednisolone acetate 1% or dexamethasone 0.1% being commonly used as go-to choices for acute unilateral NIU.31 Strategies for steroid regimens vary by provider, but in general a typical course involves hourly or half-hourly drops while awake for 1 week, followed by a slow taper over the next few weeks.32 Bilateral uveitis can indicate a more chronic or systemic disease involvement and should be treated with oral prednisone as first-line therapy, dosed at least 0.2 mg/kg/day. If necessary, stepwise therapy with cyclosporine and antimetabolites and then biologics should be pursued for bilateral cases.
While topical CS demonstrate efficacy in treating mild cases of macular oedema (ME) associated with anterior uveitis, there is no evidence to suggest that a drop regimen is appropriate for more severe cases of uveitic ME due to penetrative limitations of ophthalmic drops. The short-acting nature of topical steroids is commonly associated with the recurrence of oedema if discontinued before at least a few weeks of treatment.33 Unilateral NIU with persistent ME should be treated with oral prednisone. Parabulbar or subtenon injection of triamcinolone can be considered for patients who are at low risk of glaucoma, are aphakic or have an iris-fixated lens.34
Intravitreal corticosteroid implants
The dexamethasone 0.7 mg intravitreal biodegradable implant (OZURDEX®, Allergan, Irvine, CA, USA), designed to last up to 3–6 months, is widely used to treat uveitic ME, diabetic ME refractory to anti-vascular endothelial growth factor and ME associated with retinal vein occlusion. It is particularly useful for patients who are elderly, are pseudophakic, are vitrectomized or have no history of ocular hypertension (OHT).34 The HURON trial (cHronic Uveitis evaluation of the intRavitreal dexamethasONe implant; ClinicalTrial.gov Identifier: NCT00333814) showed OZURDEX to be effective in treating posterior uveitis.35 At 26 weeks, 23% of eyes treated with 0.7 mg required intraocular pressure (IOP)-lowering medications. Cataract development was 15%, but this was not statistically significantly greater than in the sham group. The study population at the time included only patients who were either previously or currently on another CS and/or immunosuppressive therapy. Studies on OZURDEX used as monotherapy in a study population of uveitic eyes without prior or current treatment remain sparse. One study, using a small retrospective cohort without previous systemic immunomodulation therapy, showed the efficacy of the implant in improving BCVA, decreasing central subfield thickness (CST) and maintaining IOP in eyes with ME associated with nonanterior NIU.36 Long-term studies on OZURDEX for uveitic ME show favourable outcomes in BCVA, central retinal thickness (CRT), inflammation control and decreased need for systemic CS therapy.37–39
Sustained-release fluocinolone acetonide implants, such as RETISERT® (Bausch & Lomb, Rochester, NY, USA), ILUVIEN® (Alimera Sciences, Alpharetta, GA, USA) and YUTIQ® (EyePoint Pharmaceuticals, Watertown, MA, USA), are available and hold advantages over OZURDEX due to their much longer-acting duration and propensity to achieve nearly a zero-order reaction. These medications are encased and delivered from a nonbiodegradable medium.
RETISERT 0.59 mg is designed to provide sustained release for up to 30 months. It is an intravitreal implant requiring conjunctival peritomy and full-thickness scleral incision for placement. The MUST trial (Multicenter Uveitis Steroid Treatment; ClinicalTrials.gov Identifier: NCT00132691) was a randomized study to compare the efficacy of the 0.59 mg intravitreal fluocinolone acetonide implant with that of systemic CS therapy. Results at 2 years favoured the steroid implant regarding mean visual acuity, inflammation control and macular thickness improvement.40 Observations at 7 years were less favourable compared with systemic CS therapy, but this was heavily influenced by attrition bias, lack of implant replacement, undertreatment and not incorporating crossover treatment in analysis.41 OHT was a major adverse effect, with half of the patients needing IOP-lowering medications after 34 weeks with treatment and approximately one in three patients requiring filtering surgery after 2 years.42 In a follow-up study of the MUST trial, the risk of the RETISERT pellet dislodging or separating from its original structure, causing visual disturbances, becomes more significant around the 5–6-year mark postimplantation.43 However, this issue appears preventable with timely replacement of the implant.44,45
ILUVIEN was approved by the US Food and Drug Administration (FDA) for the treatment of diabetic ME and by the UK National Institute for Health and Clinical Excellence for managing NIU of the posterior segment. The 0.19 mg implant consists of a 3.5 mm-long nondegradable case containing the active compound designed to last 36 months. It is administered via intravitreal injection using a proprietor injector, with repeated injections expected to leave behind the small encasement. ILUVIEN offers a smaller dosage and compact size and does not necessitate surgical administration, making it highly favoured for the prevention of posterior uveitic flares. At the time in which this review was written, ILUVIEN has not been approved for treating uveitis in the USA. Multiple studies have shown its effectiveness in achieving both visual and anatomical endpoints in eyes with NIU.46–52 One study suggests that the factors associated with effectiveness include female sex and a thicker retinal nerve fibre layer.52 One randomized trial (ClinicalTrials.gov Identifier: NCT01694186) showed that at 3 years, 42.5% of eyes treated with 0.19 mg of fluocinolone acetonide required IOP-lowering medications and 5.7% required IOP-lowering surgery, displaying a more favourable side-effect profile than what was seen for RETISERT.53 A retrospective case review of 13 eyes with posterior NIU through 3 years shows significant, sustained improvement in BCVA, CRT decrease and vitritis resolution with stable IOP.54
YUTIQ is an injectable therapy, similar to ILUVIEN, containing 0.18 mg of fluocinolone acetonide encased in a 3.5 mm form factor intended to provide a 36-month duration of action. This was also designed to supersede RETISERT by delivering a smaller dosage with a reduced burden of adverse effects. FDA approval was secured based on initial findings from two randomized, double-blinded, multicentre clinical trials comparing the efficacy and safety of 0.2 mg fluocinolone acetonide (designed to be released 0.2 μg/day) with sham control (ClinicalTrials.gov Identifiers: NCT01694186 and NCT02746991).53,55 Three-year outcomes favoured the implant over sham injection, showing reductions in uveitis recurrence, adjunctive therapy usage and central foveal thickness and improvements in BCVA. Similar outcomes were observed when comparing treated eyes with their untreated fellow eyes.56
Suprachoroidal delivery of triamcinolone acetonide
More recently, triamcinolone acetonide (TA) (XIPERE®, Bausch + Lomb, Laval, Canada) can be administered via suprachoroidal injection. XIPERE is the first FDA-approved therapy to be administered through the suprachoroidal space (SCS) and is indicated for ME associated with noninfectious uveitis. Delivery through the SCS allows for substantial concentration, targeted tissue exposure and higher bioavailability in posterior structures than other injection routes.57 The molecular size of the drug prevents it from being cleared through the sclera and choriocapillaris, resulting in limited exposure to the anterior segment and other body systems. The PEACHTREE trial (Suprachoroidal Injection of CLS-TA in Subjects With Macular Edema Associated With Non-infectious Uveitis; ClinicalTrials.gov Identifier: NCT02595398) showed greater efficacy compared with sham in improving BCVA, decreasing CST and decreasing the need for rescue therapy with a CS or a nonsteroidal anti-inflammatory drug (NSAID).58 IOP increase and cataract formation through 24 weeks were comparable between the two groups. No studies have compared the efficacy of suprachoroidal TA and intravitreal TA in the treatment of uveitic ME; however, studies comparing the two routes for diabetic macular oedema show comparable results, with a preference for suprachoroidal administration due to decreasing posterior thickness and having longer-lasting therapeutic effects.59,60
Addressing ophthalmic adverse effects of steroids
Despite therapeutic efficacy, steroid therapy is not without challenges, notably for its proclivity for elevated IOP and the development of cataracts. CS are thought to decrease uveoscleral outflow by inhibiting the degradation of extracellular matrix material in the trabecular meshwork (TM) through inhibition of proteases and phagocytosis, thus leading to the aggregation of material and increased outflow resistance.61 The response may involve the alteration of mucopolysaccharide metabolism, causing their accumulation in the TM. Glucocorticoid receptors are concentrated in ocular tissue, and steroids induce structural and functional changes in TM cells, affecting nuclear size, DNA content and extracellular matrix deposition.62 Approximately one in three of the general population are ‘steroid responders’, in which IOP significantly increases (5–15+ mmHg) secondary to CS treatment.63 Eyes with prior history of glaucoma are more likely to be steroid responders, develop secondary OHT earlier and require additional pressure-lowering drops.64,65 Studies have shown a positive correlation between CS potency and both severity and speed of onset of OHT.66,67 Risk factors for developing OHT in untreated eyes with NIU include previous history of OHT, systemic hypertension and AC structural irregularities, while bilateral presentation and prior hypotony are associated with diminished risk of OHT. Spontaneous normalization of IOP can be achieved post-treatment cessation.68,69 For patients with high susceptibility of being steroid responders, potent steroid alternatives with less risk of elevated IOP, such as fluorometholone 0.1%, although typically more expensive than prednisolone or dexamethasone formulations, can be a favourable choice.66,70
It is well acknowledged that uveitic eyes have an appreciable risk of developing cataracts due to CS treatment and/or chronic inflammation. Glucocorticoids bind to proteins in the lens, causing structural instability and damage in the setting of oxidation.71 It is estimated that the incidence in which a cataract develops in eyes with anterior uveitis is 5.4%.72 For intermediate uveitis, the incidence was calculated to be 7.6%.73 Topical CS were associated with an increased risk of developing cataracts only in mild cases with cell grades of ≤0.5 but not in eyes with cell grades of ≥1+.72 Steroid therapy was highly associated with cataract development if the regimen was 2+ drops per day, 4+ periocular injections or >7.5 mg oral tablet per day, whereas regimens below those dosages posed greater risk but not to statistical significance.72,73 For uveitic eyes, risk factors in developing cataracts needing surgical intervention include the exam findings at initial presentation: IOP >21 mmHg, cataract, keratic precipitate, posterior synechiae, vitritis and epiretinal membrane.73,74 Other risk factors include age >18 years, female sex, prior pars plana vitrectomy (PPV) not for retinal detachment and eyes that require glaucoma surgery.
Cycloplegics and mydriatics
The multiple purposes of topical cycloplegics in the current management of uveitis should not be overlooked. The management of ocular pain and discomfort at presentation should be the initial priority after a thorough examination. Many teaching institutions discourage the use of these drops, as mydriasis can abate flare and increase cell presence in the AC, making them difficult to appreciate on slit-lamp examination.75,76 Commonly used drops such as atropine 1% and cyclopentolate 1% are antimuscarinics that inhibit the contraction of the iris sphincter muscle, allowing the iris radial muscles to contract and move away from the pupil centre. The cycloplegic effect of paralysing the ciliary muscles prevents ciliary body spasm and, therefore, reduces the pain associated with ongoing inflammation.77 Perhaps the most important use of cycloplegics is to facilitate cleavage of synechiae via mydriasis and prevent the formation of new adhesion bodies by preventing protein leakage through the blood-aqueous barrier.78 Cyclopentolate, a short-acting cycloplegic, can promptly allow the movement of the iris to cleave synechiae or reduce their development. Both anterior and posterior synechiae are especially troublesome due to the risk of secondary glaucoma. Prompt intervention is beneficial in preventing this high-risk complication, which would otherwise necessitate surgery to resolve.
Nonsteroidal anti-inflammatory drugs
Topical NSAIDs, such as ketorolac 0.5%, bromfenac 0.09% and nepafenac 0.1%, may offer alternative options due to the side effects of CS therapy, especially for those with a history or at high risk of glaucoma. These are commonly used to treat cystoid macular oedema following cataract surgery. Topical NSAIDs are not considered first-line treatment for uveitis, and literature is sparse in this arena. One retrospective single-centre study showed that celecoxib and diflunisal prophylaxis could decrease flares in AAU, especially in cases where the patient is positive for HLA-B27.79 Likewise, literature on the efficacy of NSAIDs in treating uveitic ME is limited, with small studies showing improvement in primary endpoints with topical NSAIDs.80–82
Steroid-sparing systemic immunomodulatory therapy
Stepwise therapy includes steroid-sparing immunomodulation in cases where local or systemic CS therapy fails to elicit an adequate response or if ocular or systemic adverse effects are unacceptable. Other considerations include the presence of exudative retinal detachment, disease in the posterior pole and vision-threatening presentations.83 In children, such immunomodulation should be considered in cases involving glaucoma, cataract, ME, band keratopathy, hypotony and rubeosis iridis. Steroid-sparing immunomodulators are generally not used as first-line treatments for inflammatory processes limited to the eye, except in cases of birdshot chorioretinopathy, where CS combined with steroid-sparing immunomodulation is routinely considered.84 The various medications available have different indications, depending on the underlying disease. For advanced steroid-sparing immunosuppressants, such as azathioprine, cyclosporine, methotrexate (MTX), mycophenolate mofetil, adalimumab and infliximab, patients should be referred to a rheumatologist or a uveitis specialist. The discussion of numerous steroid-sparing immunosuppressants falls outside the purview of the expertise of ophthalmologists and the scope of this review article. Nevertheless, a select number of drugs within this category, while not approved by the FDA for treating uveitides, have options to be administered through ophthalmic routes. It is beneficial to recognize and discuss the findings pertaining to these drugs in the existing literature.
Investigative immunomodulation therapies
Topical cyclosporine is used for the treatment of keratoconjunctivitis sicca (dry eye disease) and vernal keratoconjunctivitis. Topical cyclosporine is considered to be an inappropriate approach to uveitis due to its limited intraocular penetration, fear of systemic toxicity and wide availability of topical and systemic CS.85 However, there remains potential for such topical nonsteroidal immunosuppressants to be available to ophthalmologists due to their surface application and limited systemic involvement.86 A single-centre, retrospective study compared two time periods in eight patients with recurrent anterior uveitis being treated with either topical CS, oral CS or topical NSAIDs and found that the average number of uveitic episodes per year and the duration of episodes statistically significantly decreased during the time period when patients were using topical cyclosporine.87 A mouse model study showed that topical cyclosporine delivered using microemulsion resulted in significantly reduced vision loss, intravitreal immune cell infiltration and overall clinical pathology in uveitis-induced mice eyes when compared with control.88 An intracanalicular sustained-release insert carrying cyclosporine was tested in beagles and showed no ocular and systemic toxicity over 90 days.89 Future randomized controlled trials are necessary to fully elucidate the safety and efficacy of topical cyclosporine in an ophthalmic setting.
Tacrolimus administered via the ophthalmic route has been investigated in preliminary animal studies as a potential therapeutic option for uveitis.90–92 The disadvantages of topical tacrolimus are similar to those of topical cyclosporine. It is not approved by the FDA for treating any ophthalmic conditions but has been used off-label for treating allergic conjunctivitis and uveitis. Tacrolimus exhibits limited penetration through the corneal epithelium and has suboptimal retention on the ocular surface.93 Tacrolimus has also been studied to optimize penetration through nanodelivery methods, such as microemulsions and liposomes, which have shown sustained intraocular bioavailability and reduced local toxicity.94–96 Intravitreal delivery of tacrolimus has also been explored in animal studies, demonstrating efficacy in suppressing inflammation and maintaining posterior anatomy, with little to no systemic effects.90,97,98 Although ophthalmic tacrolimus has been explored in human studies for ocular surface diseases, clinical investigations specifically addressing its application in uveitis remain absent, thus giving way for future research to address this gap.
Intravitreal and subconjunctival (SCJ) administration of sirolimus has been investigated in preclinical animal studies, showing no short-term ocular toxicity after single injections and acceptable intraocular retention.99–101 The SAKURA study (Study Assessing Double-masked Uveitis Treatment; ClinicalTrials.gov Identifier: NCT01358266), a 6-month randomized study, evaluates the efficacy and safety of intravitreal sirolimus, given every other month for noninfectious posterior uveitis at escalating doses of 44, 440 and 880 μg, with 44 μg serving as the active comparator.102,103 The 440 μg group exhibited more favourable outcomes in vitreous haze (achieving a haze score of 0 or 0.5+), faster resolution and higher success rates in achieving a complete tapering from CS therapy. BCVA change was similar across all groups. Overall, the 440 μg dosage proved particularly effective in individuals with nonanterior NIU. Most study participants have maintained or improved visual acuity. The majority also did not require rescue therapy. All three groups shared similar rates of adverse events ranging from ~16 to 20%, most of which were attributed to natural progression of disease rather than the study intervention itself. The efficacy and safety of intravitreal and SCJ sirolimus were evaluated in the SAVE study (Sirolimus as a Therapeutic Approach for UVEitis; ClinicalTrials.gov Identifier: NCT00908466).104 At the 1-year mark, both the intravitreal and SCJ treatment groups, respectively, exhibited improvement in vitreous haze outcomes in 71% of participants who had active nonanterior NIU. For all participants, visual acuity was improved by 1+ lines in 36%, maintained in 43% and worsened by 1+ lines in 21%. Numerically, from baseline, central macular thickness decreased in the SCJ group but increased in the intravitreal group. In those receiving CS therapy, the proportion of patients needing to be on >10 mg/day drastically decreased by month 12.
Intravitreal MTX has shown potential clinical utility in the treatment of retinoblastoma and ocular lymphoma.105 A small case series showed improved visual acuity across nine patients with uveitis.106 A larger multicentre case series demonstrated that intravitreal MTX improves visual acuity and reduced inflammation in 30 of 38 eyes. For patients already receiving CS therapy, MTX can contribute to a reduction in the required CS dosage. MTX underwent a head-to-head study against retrobulbar triamcinolone where it displayed noninferiority in improving vitreous inflammation and BCVA in patients with posterior uveitis associated with Behçet’s disease.107 The findings also indicate that MTX results in fewer relapses. The MERIT trial (Macular Edema Ranibizumab v. Intravitreal Anti-inflammatory Therapy; ClinicalTrial.gov Identifier: NCT02623426) demonstrated that 400 μg intravitreal MTX was inferior to a 0.7 mg dexamethasone implant in the treatment of persistent and recurrent uveitic ME.108 The MTX-treated group showed improved CST but unchanged BCVA. MTX had a lower propensity for significant IOP elevations and fewer incidents requiring IOP-lowering medications compared with dexamethasone. Various investigations, including retrospective studies and case reports, highlight concerns about the toxic effects of ophthalmic MTX on the corneal epithelium; however, topical lubricants, topical immunosuppressants and decreasing the frequency of injections have been shown to adequately address this adverse effect.109–113
Surgery
Intraocular surgical intervention can be a useful therapeutic and/or diagnostic approach for managing NIU, especially in cases that are refractory to medical therapy or involve specific complications secondary to chronic inflammation. Although no formal indications exist, therapeutic indications may include, but are not limited to, vision-occluding media opacities of the cornea, lens or vitreous body; lens-induced uveitis; posterior structural complications; hypotony and the need for therapeutic device implantation. Preoperative measures to reduce inflammation or maintain adequate immunosuppression for a minimum of 3 months before surgery should be considered as intraocular manipulations can worsen the disease.114
Uveitis can lead to the development of cataracts, and conversely cataracts can induce uveitis through an autoimmune response triggered by phaco-antigens. Cataract extraction is commonplace to address these issues and to properly assess uveitic involvement of the posterior pole. In cases with synechiae, incorporating synechiolysis and using pupil-dilating devices prior to capsulorhexis and phacoemulsification are beneficial.115 Studies suggest that hydrophobic acrylic intraocular lens are less likely to result in posterior synechiae and overall exhibit better compatibility with uveal structures than IOLs of hydrophilic material.116,117
Band-shaped keratopathy is commonly observed in JIA-associated uveitis, and it should be met with intervention, especially in those at an age susceptible to amblyopia. Treatment involves removing calcified bodies through keratectomy or chelation with ethylenediaminetetraacetic acid.
Secondary glaucoma is estimated to occur in approximately one in five patients with uveitis, and of those affected 10–20% may need surgical intervention.118–120 For decades, trabeculectomy has been the gold standard approach for rapidly progressing glaucoma, favoured for its ability to address the condition without requiring an additional implant or device.121 In uveitic glaucoma, trabeculectomy may be at risk of failure due to fibrosis of the manipulated tissue, thus causing bleb closure, especially considering the chronic inflammation and age of these eyes.122–124 An Ahmed valve placement is one of the most widely used surgical approaches for glaucoma and is a common approach in uveitic glaucoma. One-year outcomes show similar success rates between trabeculectomy with mitomycin C and Ahmed valve implantation in eyes with glaucoma secondary to uveitis.125 The placement of a Baerveldt shunt, as opposed to an Ahmed valve, presents as a favourable alternative with lower failure rates in uveitic glaucoma and may be preferred for eyes requiring more aggressive IOP management.126 A review article comparing 1-year outcomes of trabeculectomy, Ahmed valve and Baerveldt shunt showed comparable IOP reduction, visual acuity changes and varying number of topical pressure-controlling drops across the three approaches, with Baerveldt shunt having a significantly lower failure rate.127
PPV is performed for both diagnostic and therapeutic purposes in the surgical management of severe cases of uveitis. Findings that may require diagnostic vitrectomy are nonresponsiveness to immunosuppression, rapidly evolving diseases with inconclusive workup, ocular malignancy or other severe atypical presentation. Techniques available in diagnostic vitrectomy include vitreous biopsy and chorioretinal biopsy.114 As opposed to a vitreous tap, a mechanized vitreous biopsy allows for larger sampling to be completed. This is done via three-port PPV and air infusion for IOP control. A 20-, 23- or 25-gauge cutter is used and can be safely used at up to 15,000 cuts per minute without compromising cell viability.128 Maximizing yield volume and quality while minimizing vitreous disturbance is a primary objective, especially in intraocular inflammation-prone uveitic eyes that are vulnerable to iatrogenic complications. Microincision vitrectomy surgery is increasingly favoured in such cases due to its capacity to achieve comparable outcomes with reduced incision size, decreased surgical duration, instrument manoeuvrability and improved IOP control.129 While preoperative inflammation control is beneficial for surgical outcomes, this is not required prior to PPV to ensure adequate diagnostic yield and timely treatment. Irreversible vision loss in uveitis is most commonly due to chronic ME and scarring.130 PPV can be beneficial in treating such uveitic posterior complications as well as vitreous haemorrhage, epiretinal membrane, cyclitic membrane and retinal detachment. Therapeutic effects of PPV in uveitic eyes for intraocular inflammation have been reported.130–133 Evidence shows improved BCVA, decreased inflammation, decreased frequency of flare-ups and decreased steroid therapy burden.
Referral to ophthalmology or uveitis specialist
In real-world settings, patients may initially present with uveitis to their primary physician or optometrist. Minor inflammatory symptoms of the eye account for 1% of primary care visits, much of which consist of conjunctivitis.134 Without basic ophthalmic equipment, major differentiating factors cannot be used to differentiate between uveitis and conjunctivitis. Photophobia, pain, significant decrease in visual acuity, persistent inflammation and history of autoimmune disease align more with the former, and purulent or watery discharge, itchiness, recent sinusitis and periorbital oedema align more with the latter. Without the means for a thorough eye examination, a referral to an ophthalmologist or optometrist, depending on geographical location and resources, should be prompt in the setting of ocular inflammation. Optometrists can evaluate, diagnose and initiate treatment with topical steroids and cycloplegics for AAU.135 If the presentation is not that of AAU, the posterior chamber cannot be visualized, or if the improvement is not noted with the initial treatment, patients should be urgently referred for specialist care.136 Referring physicians are encouraged to look up members from the following societies for uveitis management: the American Uveitis Society, the American Association of Ophthalmologists, and the Ocular Immunology and Uveitis Foundation. Members of these societies are self-designated as having an interest in uveitis.
To assist in diagnosis, referral process and patient outcomes, the SUN working group anatomical classification, descriptors, grading scheme and terminology should be used.137 While this classification has existed since 2005, many nonspecialists have yet to ultimately adopt it into their evaluation. In a study of 315 patients referred to a uveitis specialist, 37.4% of referrals had no uveitis classification; of those that did, 48.1% were incomplete.138 Referral to a uveitis specialist is ideal to ensure appropriate disease management. Upon reviewing treatments from referring providers in Colombian health centres, 65% of patients were appropriately treated with topical steroids and 41% were appropriately treated with systemic therapies.138 Meanwhile, in Canadian health centres, 48% were appropriately treated with topical steroids and 10% were appropriately treated with systemic treatments.139
In 2022, there were approximately 174 uveitis specialists in the USA, highlighting the scarcity and geographical dispersion of uveitis care.140 Delays in diagnosis and treatment can be detrimental to vision. A correlation between referral time and complications, as well as visual impairment, has been described in a paediatric population with uveitis.141 One study found that the mean time for uveitis speciality appointments was 108.5 weeks.138 Paediatric evaluation by uveitis specialists has shown a similar wait time.141
Referral to rheumatology
NIU is highly correlated with autoimmune diseases and should be subsequently referred to a rheumatologist if not already under their care. In one study of patients referred to rheumatological clinics, half of NIU cases were associated with spondyloarthritis; the remaining were associated with Behçet’s disease (13.9%) and idiopathic aetiology (9.2%).142 A study of children diagnosed with NIU demonstrated that 20–25% of diagnoses were associated with JIA.143 Uveitic patterns may guide practitioners’ suspicion towards the underlying rheumatological disease. Patients with psoriatic arthritis had primarily acute courses with unilateral involvement compared with those without psoriatic arthritis. Similarly, uveitis involvement in patients with rheumatoid arthritis was mainly anterior and unilateral. Patients with Behçet’s disease were found to have a bilateral posterior involvement, as well as being more prevalent in males. Meanwhile, idiopathic NIU was predominately anterior and bilateral.142,144 However, one cannot use the subtype of uveitis as an indication to refer or not to refer, as various autoimmune processes present in different or multiple areas of the uvea.145–147
Patients should be referred to a rheumatology clinic to manage the underlying autoimmune disease process further and prevent the recurrence of ocular symptoms. For example, early management of JIA-associated uveitis with MTX and adalimumab has been shown to reduce uveitis recurrence and topical steroid burden, as demonstrated in the SYCAMORE study (Safety and Cost Effectiveness of Adalimumab in Combination with Methotrexate for the Treatment of Juvenile Idiopathic Arthritis Associated Uveitis; EudraCT number: 2010-021141-41).148 Another study of patients with NIU referred to rheumatological clinics showed that 90% received systemic therapies.149 In an adult population with Behçet’s disease, intensive management showed that visual prognosis was significantly improved, with only 2% of patients developing blindness at 6 years of follow-up.150
An interdisciplinary approach to patients presenting with NIU can offer earlier workup for systemic symptoms and earlier diagnoses of the underlying disease with subsequently improved medical management.151 A review of systems should be considered for dermatological, gastrointestinal, genitourinary, musculoskeletal and respiratory systems.136 Ophthalmologists and rheumatologists have established standardized criteria for identifying concerning findings in patients with uveitis that warrant a rheumatological referral.152 In the setting of NIU, these ‘red flags’ include chronic low back pain, joint symptoms in a child and family and/or personal history of psoriasis, spondyloarthritis, inflammatory bowel disease, Behçet’s disease, oral or genital aphthae or erythema nodosum.
Discussion
The management of uveitis presents a nuanced challenge, requiring simultaneous treatment of acute-onset episodes, prevention of recurrences and monitoring for adverse effects. Predominantly, CS therapy serves as the cornerstone of treatment for NIU from an ophthalmic perspective, although concerns over side effects, such as OHT and cataracts, remain significant, particularly when surgical intervention becomes necessary. Given the chronic and recurrent nature of NIU, there is a growing reliance on longer-acting CS formulations to provide sustained suppression of inflammation. However, the management of long-term systemic immunosuppression poses numerous challenges, especially within the ophthalmic context. In this regard, intraocular steroidal implants offer a promising avenue for localized immunosuppression, but these require periodic replacement and are associated with increased risks of OHT and cataracts. The structural design of these implants plays a crucial role in determining their efficacy and the potential for complications upon replacement. Moreover, in cases of uveitic glaucoma or implant-induced glaucoma, a combination of extended-release steroidal implants and filtration surgery synergistically contributes to effective IOP control.153–156 Identifying suitable candidates for intraocular implants is paramount, as direct intraocular involvement poses a higher risk of increased IOP and cataract formation compared with medication administered topically. Additionally, nonsteroidal immunomodulators delivered via ophthalmic routes show promise in controlling inflammation with fewer associated risks of IOP elevation. Although their topical delivery is hindered by limited surface penetration, nanodelivery systems such as microemulsions offer a potential solution to enhance their efficacy. Furthermore, while intravitreal delivery of nonsteroidal immunomodulators holds potential, further head-to-head studies comparing their efficacy against intravitreal steroidal therapy are warranted.
Given the high prevalence of underlying autoimmune diseases in patients with uveitis, there is a necessity to develop long-term therapeutic strategies to prevent recurrences, particularly in cases involving posterior structures that can lead to ME and subsequent visual deterioration over time. Chronic uveitis imposes a long-term burden on visual and intraocular surgical outcomes.157 Therefore, cases of recurrent and refractory uveitis, especially those involving posterior structures, benefit from a comprehensive evaluation and referral to rheumatologists for further diagnostics and potential systemic therapy. Uveitis is uniquely challenging, as ophthalmologists are not comfortable with systemic immunosuppression, and rheumatologists are not as comfortable with ocular anatomy and lack specialized equipment for a full ocular examination. This multidisciplinary approach is crucial in complicated and recurrent cases, as highlighted in the Fundamentals of Care for Uveitis Initiative.83