Current Therapy of Retinal Vascular Disease
Retinal vascular disorders are commonly found in ophthalmological practice: in addition to hypertensive changes and retinal vein occlusions, diabetic eye disease play a major role. Driven by demographic change and the obesity trend, the prevalence of diabetes has increased steadily over the last years and is likely to rise further. Diabetic retinopathy (DR) and diabetic macular oedema (DMO) are ocular complications of diabetes, where numbers are expected to double by 2030.1 As opposed to other retinal diseases, DR and DMO frequently affect the working age population, requiring long-term disease management. To date, DR and especially its manifestation DMO is the main cause of severe visual impairment and blindness.1–4
For many years, laser photocoagulation has been the mainstay in the treatment of proliferative DR (PDR) and DMO.5,6 For PDR panretinal laser photocoagulation (PRP) is the method of choice to repress neovascularisation caused by retinal ischaemia and to prevent serious complications. Likewise, for DMO without foveal involvement focal laser has been the gold standard for the last three decades.6,7
The concept of clinically significant macular oedema (CSMO) was introduced by the Early Treatment Diabetic Retinopathy Study (ETDRS), describing a thickening of the retina and/or hard exudates within a distance of 500 μm from the fovea or a zone of oedema greater than one disc area at a distance of one disc diameter of the fovea.6 Even though the patient still has good vision, immediate action is warranted. Numerous studies have shown that a significant stabilisation of visual acuity can be achieved in patients with CSMO by a single or repeated focal laser treatment.3,4,7
While the exact mechanisms of action of laser photocoagulation in DMO (focal or modified grid laser photocoagulation) are not fully understood, it seems clear that extensive tissue scarring is not the primary aim as it is in laser retinopexy or panretinal laser treatment for PDR. It has been postulated that a major goal of macular laser therapy is to solve leakage arising from macular vessels by photocoagulating photoreceptors and it is believed that in macular laser treatment, photocoagulation of photo receptor outer segments results in sealing of the blood vesselsin the area of highest visual acuity and the subsequent reduced oxygen demand of the outer retina helps reduce retinal hypoxia.8–10 In addition,increased oxygen tension in the inner retina helps to decrease tissue oedema and improve vision by autoregulatory vasoconstriction and reduced hydrostatic pressure in the capillaries and venules.8,10
With a delayed onset-of-action, treatment success after macular laser photocoagulation can be assessed at the earliest 3 months after the therapy session.11 Three to four treatments are typically required when using a slit-lamp-based, manually applied laser to achieve stabilisation of vision.11 On average, only limited visual gains can be expected.6 Over the years, the original ETDRS laser protocol was steadily adjusted and improved, leading to the modified ETDRS protocol used for example in the more recent studies of the Diabetic Retinopathy Clinical Research Network (DRCRnet).8 However, it was found that despite these improvements to the original protocol, no significant visual improvement could be reached with conventional laser therapy. This holds true also and especially for clinically significant DMO, where the centre of the eye’s sharpest vision is involved.
By contrast, the easy-to-standardise pharmacological therapies such as intravitreal anti-vascular endothelial growth factor (VEGF) injections could demonstrate rapid onset-of-action and overall convincing results even over long periods of time (3 years and beyond).5,12,13 Therefore, in many countries around the world centre-involved DMO is treated with a pharmacological regimen as first-line therapy. In this indication ranibizumab (Lucentis®, Novartis/Genentech) has been approved in Europe and the US, following long-term off-label use of bevacizumab (Avastin®, Genentech). Both drugs bind to VEGF as an antibody fragment/ antibody and act as inhibitors of VEGF signaling in the retina. Particularly for ranibizumab, long-term visual stabilisation and even an improvement by one or two ETDRS lines on average could be demonstrated in prospective, randomised, multicentre trials.5,13,14 These trials have also shown that regular/repeated intravitreal application is required for lasting success. Typically seven to nine, but up to 12 injections accompanied by intensive (monthly) diagnostic monitoring were necessary in the first year of therapy.5,13,14 Compared with the three to four sessions of laser photocoagulation applied in the past, this places a significantly higher burden on patients, doctors, clinics and healthcare systems.
Although not fully conclusive in this respect, the studies plausibly indicate that a combination of initial anti-VEGF therapy and subsequent laser therapy may help reduce the number of injections while maintaining visual stabilisation or improvement.5,15,16 In the DRCR.net Protocol I study, the best results were achieved in patients receiving injections first and focal laser 6 months later (‘deferred laser’ arm).5 In addition, the recently published three-year results of the Ranibizumab for Edema of the Macula in Diabetes (READ-2) study show that the combination of anti-VEGF andmacular laser therapy required the least number of anti-VEGF injections without significantly compromising visual outcome.12
Therefore, it appears as the next logical step to combine the positive results of pharmacological therapy with the sustained effect of the laser treatment, backed by decades of experience, to further improve management of DMO. Potentially, such a combination regimen could reduce macular oedema with a few anti-VEGF injections and stabilise the positive result with a single laser treatment. However, the demands regarding the accuracy and completeness of laser treatment are particularly high. The physician must have full confidence in the laser treatment chosen to avoid rebound oedema and possible visual loss as a consequence when pausing anti-VEGF treatment.
Navigated Laser Therapy
One major challenge in conventional laser photocoagulation treatment of retinal disease is to achieve precise application of laser energy to microaneurysms and areas of oedema. The physician has to manually apply the laser spots from her or his recollection of the diagnostic image and only basic planning is possible – limitations that have not been overcome by even the most recent advances to slit-lamp based systems. A potential approach to solve these limitations may be to combine essential diagnostics and therapy in one system. First approaches were taken by companies Rodenstock (1986) and Ocular Instruments (1990), integrating film-based fluorescein angiography (FA) with slit-lamp laser photocoagulation.17,18 However, inadvertent eye movements, such as saccades and rolling movements, posed an insurmountable challenge to the contemporary technology and precluded widespread clinical adoption. Advances in information technology and image processing in the late 1990s led to more sophisticated solutions, such as the computer-based US Research System by Wright (2000), which could stabilised a treatment image under laboratory conditions – a first step towards computer-guided retinal laser therapy.19
With the technological progress of the last decade and in parallel to the rapid evolution of refractive laser surgery, a robust image stabilisation system for the posterior segment became available. Based on this, the idea of Retina Navigation was born and developed by a close collaboration between the university eye hospital of the Ludwig-Maximilians-University in Munich and OD-OS GmbH (Teltow, Germany). Following intensive preclinical and clinical development, as well as CE certification and US Food and Drug Administration (FDA) clearance, the Navilas System (ODOS) was introduced as the first laser photocoagulator introducing Retina Navigation to the clinic. Navilas integrates fundus imaging, including truecolour and FA with computer-based image-guided retinal laser therapy.20 Both digitally planned treatments and navigated pattern laser treatments can be performed to completion at high accuracy.20
Navigated treatments in the posterior pole are typically performed using the system planning features. The individual treatment plan is typically drawn on a Navilas colour image or FA that can be co-registered with external images. Examples from clinical practice include optical coherence tomography (OCT) thickness maps, external FA images including widefield, indocyanine green angiography and fundus autofluorescence. Laser spots can be placed individually and in groups on the still image and so-called exclusion zones for laser application can be defined. Figure 1 shows a treatment plan based on an external OCT image.
As soon as the plan has been generated with the patient at rest, the actual treatment can be rapidly performed to completion with computer-guidance (‘target assist’) and under infrared illumination.
During treatment, the plan is automatically overlaid onto the real-time infrared image of the fundus with and/without the original plan image displayed (see Figure 2). The aiming beam is automatically pre-positioned on the first and each subsequent treatment location, stabilised and adjusted for inadvertent eye movement. Laser application itself is controlled by a classic foot switch and titrated according to automatically obtained colour images displayed as an animation in a separate window.
Even the first clinical prototypes of Navilas demonstrated that high precision and reproducibility of the applied laser burns with a deviation of less than 100 μm from pre-planned target can be achieved, not only in vitro but also in everyday clinical situations.21
Not surprisingly, this precision combined with the controlled completion of therapy according to plan provided advantages over conventional laser. Initial case series and a case-control study demonstrated that in DMO patients navigated laser therapy could reduce the need for re-treatment by almost half compared with conventional laser monotherapy (18 % versus 31 % at 8 months).21–23 Apart from this potential reduction in the number of treatments, navigated laser also seems to provide immediate advantages to the patient.
In a recently published study, patients reported a consistently lower level of therapy discomfort versus conventional laser, owing to faster treatments after pre-planning as well as the reduction of glare by infrared illumination and the omission of the contact glass in most treatments.20,24
From the physician’s perspective, first-time users may view the careful treatment planning as an additional labour burden, while they have patients waiting. Planning, however, shortens the actual treatment time and retreatments are minimised for an overall muchmore efficient therapy.23,24
Indeed, Retina Navigation has brought transparency and standardisation to retinal laser. Our definition of a consensus therapy protocol within a panel of experts revealed surprisingly dramatic differences in the interpretation of the modified ETDRS scheme. The integration of imaging and treatment and separation of process steps now allows the demonstration, discussion and revision of treatment plans with colleagues as well as the definition of a therapy standard. This greatly benefits teaching and for the first time enables telemedicine: a plan can be e-mailed to another expert for review and applied later with or without revisions.20,25–27
Panretinal and Sectoral Laser Therapy with the Navilas Laser System
The introduction of a wide-field objective and custom contact lens has opened the system for navigated treatments of the far-periphery (see Figure 3). The dynamic field-of-view matches conventional lasers. As in navigated focal treatments, treatment can be performed under comfortable infrared illumination with spots digitally documented. Stabilisation of the aiming beam on the retina enables not only the application of fast patterns (10–30 ms pulses) known from other devices but also patterns with 100 ms and higher pulse durations as described by the ETDRS. In general, it is technically possible to perform treatment planning in the periphery as well. The overlay of wide-field FA and planned targeting of ischaemic areas is currently clinically evaluated. In current clinical practice a standard panretinal photocoagulation is typically not pre-planned, but patterns are directly placed on the live retina to save time. Initial experience from our clinic suggests that besides panretinal photocoagulation in PDR, the sectoral lasering of branch retinal vein occlusions (BRVOs) can also be performed efficiently and with high precision.
Navigated Laser Therapy for Diabetic Macular Oedema
Conditions treated with navigated laser include central-serous chorioretinopathy, choroidal neovascularisation, polypoidal choroidal vasculopathy, idiopathic perifoveal teleangiectasia and BRVO. Besides PDR DMO is the main indication for navigated laser therapy.21–23
In the past years, the use of anti-VEGF intravitreal injections, ranibizumab, bevacizumab and aflibercept, has demonstrated significant visual gains from baseline and compared with conventional laser monotherapy.14,21 Since then, anti-VEGF has pushed conventional laser aside in the management of patients with centre-involving DMO to the extent of raising the question if there is ‘still a place for laser in DMO’ among experts. As anti-VEGF has demonstrated a much more rapid onset-of-action in major trials, it is predestined as a first-line treatment to relieve oedema. However, DMO therapy with anti-VEGF is typically chronic requiring repeat monthly injections for several years to achieving optimum visual results. In this context, there may well be a place for a treatment that adds durability to anti-VEGF visual results reaches non-inferior outcomes and significantly reduces the injection burden. Not only to reduce the logistic and financial strain from doctors and healthcare system, but as not all patients will be able or willing to follow such a rigorous treatment regimen in practice.
As far as conventional laser treatment is concerned some trials, including READ-2 36-month extension data, suggest an injection-saving effect, while other major trials show no effect of laser on injections and visual outcome at all.5 While long-term experience and study results suggest a stabilising effect of laser with and without anti-VEGF, recent trials have not sufficiently addressed to answer that question.
To address these conflicting results with a more standardised and reliable laser approach, we and our collaborators from the University of California (William R Freeman and colleagues) have developed a combination therapy paradigm that is compatible with the European label and guidelines for ranibizumab and uses Navilas once patients respond to anti-VEGF. In patients with clinically significant DMO: three ‘loading’ injections are given to reduce macular oedema followed by pro re nata (PRN)/as needed injections bases on visual acuity and OCT results. Navigated laser is applied 1 month after the loading phase as a modified grid treatment. OCT and FA findings are incorporated to treat areas of retinal thickening and focal leakage, respectively.
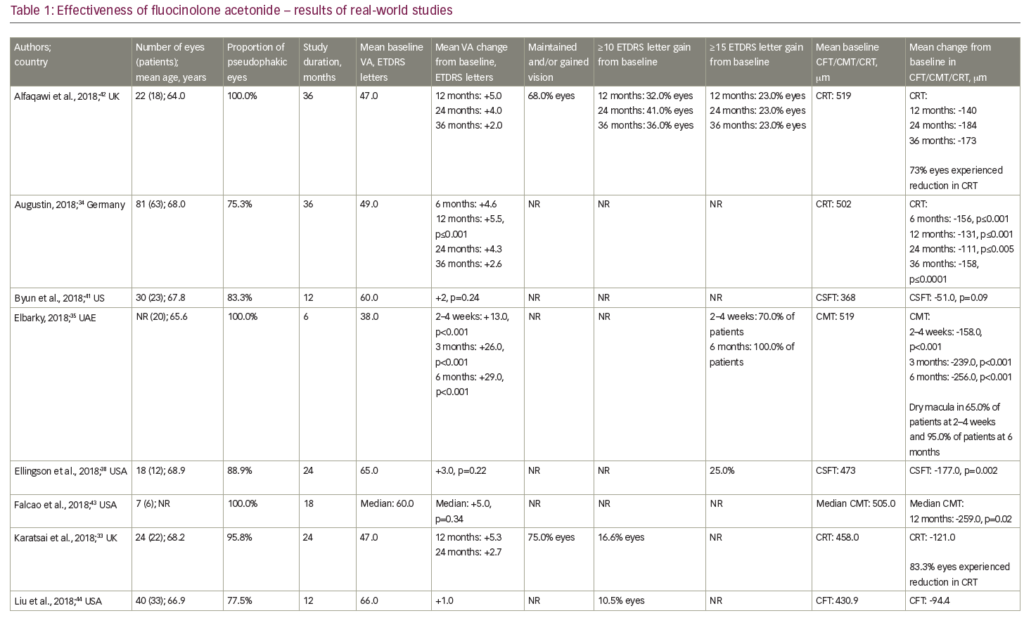
Recently, we have presented 12-months results of a pilot cohort study (n=66) comparing this regimen to ranibizumab monotherapy using the same PRN protocol (Kernt et al., AAO 2013 meeting). By month 12, combination therapy eyes had improved 8.4±8.3 letters and monotherapy eyes had improved 6.3±6.5 letters (not significant). Combination therapy eyes required 0.9 injections post-loading, while monotherapy eyes required 3.9. (difference p<0.001).
Our results are supported by a study by the University of California San Diego, based on a chart review of patients that had been treated with a similar standardised combination therapy regimen utilising Navilas and bevacizumab. In these patients, an average of four injections were necessary during 12 months follow up (preliminary results from paper presentation by Freeman et al. ‘Multicenter Evaluation of Navigated Laser to Reduce Anti-VEGF Injection Frequency in Diabetic Macular Edema (DME)’ at The Macula Society, Annual Meeting, February 27 to March 2, 2013, Dana Point, CA, US).
While randomised studies, more study centres and longer follow up are needed to finally assess this treatment scheme, this pilot study demonstrates that the combination therapy paradigm with navigated laser may allow to provide good visual outcomes and significantly reduce injection burden.
Summary
The Navilas laser system introduces computer-assisted therapy, which has long been standard in refractive laser surgery to the field of retinal photocoagulation. Both in the macular and the peripheral retina, the assistance systems of the Navilas Laser provide high precision and safety in therapy, as well as additional advantages in terms of standardisation of planning and execution. In addition, digital documentation of laser spots and parameters allow for quality assurance in retinal laser therapy.
Navilas integrates diagnostics and laser therapy in a system with a focus on the navigated therapy. Potential advantages of this technology over conventional laser become particularly obvious in focal macular laser therapy and consequently navigated laser therapy has been a primary focus as a treatment option for DMO without direct involvement of the fovea and – as a combination therapy with anti-VEGF injections – in DMO with foveal involvement.
The main goal here is to further optimise the available treatmentoptions and particularly their combination and timing to improve long-term treatment success, namely visual outcome, at the lowest number of interventions possible. Furthermore, in the treatment of peripheral retinal pathologies, the navigated laser therapy is an interesting new option.
This paper was previously published for the European audience in: European Ophthalmic Review, 2013;7(2):127–130