During ophthalmic surgery, surgical trauma causes activation of cyclo-oxygenase (COX) COX-1 and COX-2, which metabolise arachidonic acid to prostaglandins (PGs). PGs are mediators of the inflammatory response, and increased production of these molecules can result in discomfort, pain and ocular inflammation. As inhibitors of PGs, non-steroidal anti-inflammatory drugs (NSAIDs) are often employed by ophthalmic surgeons to provide anti-inflammatory control post-surgery and work synergistically with steroid therapy to minimise pain and inflammation following ocular surgery,1,2 albeit by different mechanisms. NSAIDS primarily act on cyclo-oxygenase-1 (COX-1) and COX-2 to minimise PG formation,3 and while steroids also reduce PG synthesis, this is due to the inhibition of phospholipase A2.4
Moreover, NSAID treatment has been demonstrated to have a beneficial effect on visual outcomes,5 preventing macular oedema after cataract surgery, however, it is essential to attain therapeutic concentrations in the posterior chamber to obtain the effect of NSAID treatment on the target retina tissue. Thus, for maximum therapeutic benefit, the ideal NSAID is one that reaches therapeutic levels in both the aqueous humour and in the posterior segment tissues. Nepafenac is a NSAID with a unique prodrug structure that has superior corneal permeability to other currently available NSAIDs.6 This review aims to consider the properties, existing efficacy and safety data, other possible indications of nepafenac in inflammation treatment and the advantages it provides over existing NSAIDs in cataract surgery.
Mode of Action of Nepafenac
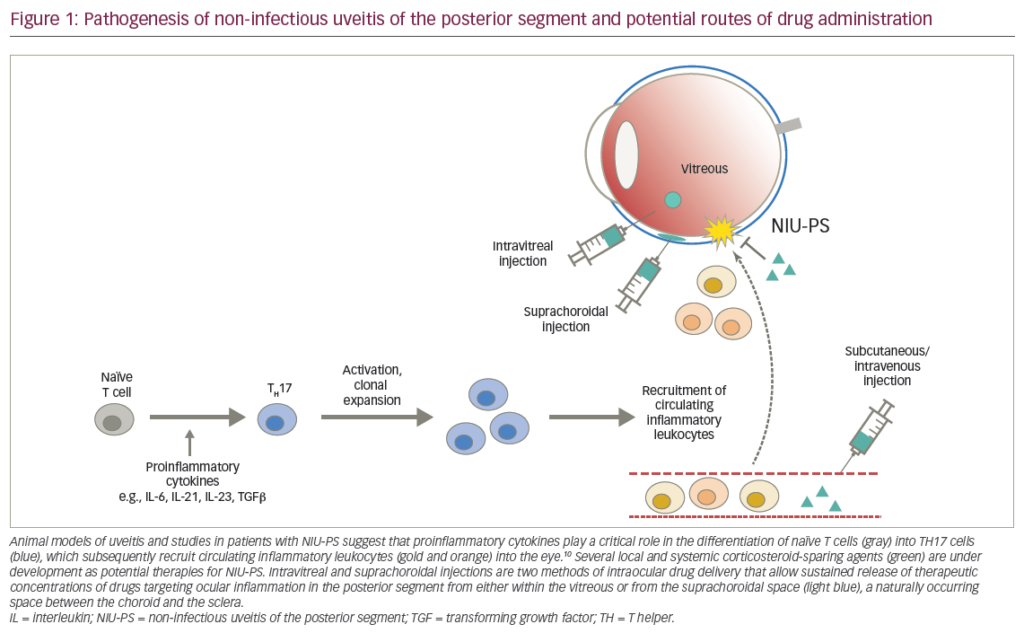
Nepafenac has a unique prodrug structure and is converted to a potent cyclo-oxygenase inhibitor, amfenac, by intraocular hydrolases (see Figure 1).6,7 Upon ocular dosing, nepafenac permeates the cornea, is metabolised by intraocular tissues8 and is converted into amfenac for optimal efficacy. The prodrug mechanism of action maximises bioactivation to amfenac in the iris, ciliary body, retina, choroid and cornea to a lesser extent, making nepafenac a target-specific NSAID.9 xperimental studies on nepafenac demonstrated properties of enhanced permeability and rapid bioactivation to amfenac, to inhibit PG synthesis in the anterior and posterior eye segments.7
To view the full article in PDF or eBook formats, please click on the icons above.