Uveal melanoma is the most common primary intraocular malignancy in adults and comprises approximately 85 % of all ocular melanomas.1 With current clinical examination techniques, the accuracy of clinical diagnosis of uveal melanoma exceeds 99 %.2 This is in sharp contrast to other systemic malignancies for which biopsy remains the gold standard for diagnostic confirmation. A variety of imaging techniques have been used for differentiating uveal melanoma from other tumours or simulating conditions.
Uveal melanoma is the most common primary intraocular malignancy in adults and comprises approximately 85 % of all ocular melanomas.1 With current clinical examination techniques, the accuracy of clinical diagnosis of uveal melanoma exceeds 99 %.2 This is in sharp contrast to other systemic malignancies for which biopsy remains the gold standard for diagnostic confirmation. A variety of imaging techniques have been used for differentiating uveal melanoma from other tumours or simulating conditions.
The primary diagnostic modalities include slit-lamp examination, transillumination, digital photography, A-scan and B-scan ultrasonography (USG), ultrasound biomicroscopy (UBM), angiography and optical coherence tomography (OCT). Slit-lamp examination of the anterior segment and dilated fundus examination with 90D and 20D lenses is useful to locate the tumour and to assess its surface characteristics and associated features. Transillumination can also be used to visualise the margins of anterior choroidal melanoma or ciliary body tumours not visible on slit-lamp examination. USG can be performed using either A-scan or B-scan and helps in the documentation of posterior tumours. UBM aids in the assessment of anterior segment tumours. Angiography, particularly indocyanine-green angiography (ICG), reveals choroidal circulation and characteristics of tumour vasculature. Lastly, newer developments in OCT allow assessment of associated features such as sub-retinal fluid, drusen or retinal atrophy.
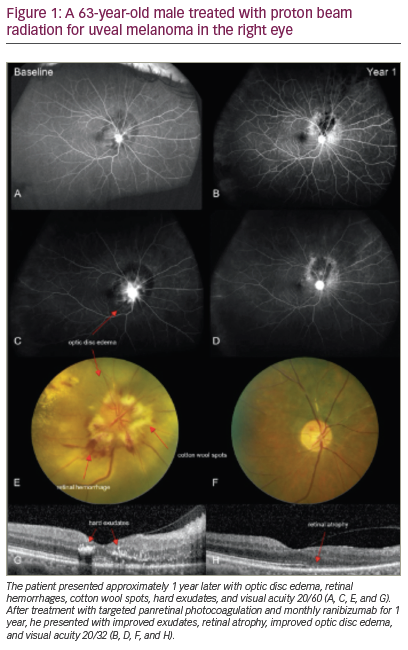
The role of ancillary studies such as computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET) (see Figure 1) and immunoscintigraphy is limited to atypical cases and surveillance for metastases.
Digital Photography
Digital slit-lamp and fundus cameras are useful for documenting the clinical features of uveal melanoma and provide a ready means for future comparison to monitor growth or response to treatment.
Iris Melanoma
Despite being the most common primary malignancy of the iris, melanoma in this location comprises only 3–10 % of uveal melanoma.3 These tumours are either diffuse or circumscribed and tend to arise in the inferior portion of the iris. Iris melanomas vary in colour from light to dark brown and rarely can be amelanotic. In lightly pigmented tumours, intrinsic vascularity is usually visible.4 When differentiating iris melanoma from nevi, features such as basal size >3 mm, prominent feeder vessels, secondary glaucoma or rapid growth are more suggestive of iris melanoma. Slit-lamp photography is useful for documenting the location and extent of tumour, tumour growth, tumour vascularity and associated features such as keratopathy, cataract or hyphema. In addition, gonioscopic slit-lamp photography is useful for documenting pigment dispersion, closure of the angle by tumour or pigment cells, or seeding of cells into the anterior chamber.
Ciliary Body Melanoma
In contrast to iris melanoma, ciliary body melanoma usually presents later in the fifth and sixth decade.4 In general, ciliary body melanoma is detected late and is associated with a poorer prognosis. For this reason, early detection is essential. These tumours present as either a circumscribed or diffuse form. At an early stage, tumours in this location are often asymptomatic and may not be readily documented with photography unless visible in the anterior chamber angle. Larger, circumscribed tumours often present with decreased vision and may be photographed following full pupillary dilatation. Other variants such as annular or ring melanoma are more difficult to detect. Sentinel vessels, neovascularisation of the iris, sectoral cataract and shallow anterior chamber are features seen in annular tumours and can be photographed with slit-lamp photography.
Choroidal Melanoma
Slit-lamp photography can be useful for documenting the anterior segment findings that are sometimes associated with choroidal melanoma such as episcleral sentinel vessels, iris hetereochromia or oculodermal melanocytosis (Nevus of Ota).
Fundus photography provides a ready means of documenting the majority of these tumours. Standard mydriatic photography captures as much as 85° of the fundus, which is not ideal when tumours are located in the periphery. Wide-angle systems are available that can capture up to 200°. Evaluation of basal diameter may be more accurate with wide-angle fundus photograph than with USG, as the shallow margins may not be detected by ultrasonography.5 Choroidal melanoma is typically dome or mushroom shaped, but can also occur as a diffuse form. They are grey to greenish-brown in colour. There may be overlying orange pigment. Choroidal melanoma may cause exudative retinal detachment and retinal pigment epithelium (RPE) changes such as necrosis or atrophy. The presence of drusen is more suggestive of nevi. In addition to recording tumour margins with respect to the retinal vessels, the software can measure lesion size to accurately monitor tumours for growth or recurrence.
Ultrasonography
Ophthalmic USG is a powerful, non-invasive and inexpensive tool that aids in the diagnosis of uveal melanoma. It uses higher frequency for better tissue resolution compared with abdominal USG for which greater tissue penetration is required.
USG can accurately define tumour location, shape, size and degree of extraocular extension, which is useful for proper staging and selection of treatment. Serial monitoring of these parameters allows for evaluation of growth or response to treatment. B-scan USG is more sensitive than CT or MRI in detecting extra-scleral extension.6
B-scan Ultrasonography
Using a frequency of 10 MHz, B-scan USG provides a 2D acoustic section of the eye and is one of the most important imaging modalities used to diagnose and evaluate choroidal melanoma. Choroidal melanoma has varied growth patterns and can be dome shaped or flat. A pathognomic finding is a ‘collar button’ or a ‘mushroom’ shaped tumour that results from a rupture through Bruch’s membrane; however, this configuration is present in only 25 % of cases. Irrespective of shape, these tumours maintain their characteristic features on USG, displaying echodensity due to the interface between tumour cells and intrinsic vessels. Near the base, an acoustic quiet zone may be observed due to relatively avascular tumour. Intrinsic vascular pulsations may be visible in some tumours. B-scan USG is also helpful in cases with dense vitreous or sub-retinal haemorrhage in which the fundus view is restricted, permitting serial examinations.
In addition to measuring the size and extent of a tumour, B-scan USG can also be used intra-operatively to confirm the position of the radioactive plaque, especially in posterior tumours where plaque placement may be technically challenging (see Figure 2).
A-scan Ultrasonography
Quantitative USG using standardised A-scan can help differentiate choroidal melanoma from other simulating entities by determining reflectivity, internal structure and sound attenuation. Reflectivity is graded by the height of the spike on A-scan compared with a zero baseline and a 100 % spike of retina and all tissues equal or higher in density. Reflectivity can only be accurately determined when the A-scan probe is directed perpendicular to the lesion. Choroidal melanoma has a low-to-medium reflectivity and a high initial spike on standardised A-scan USG (see Figure 3). Sound attenuation is often observed at the base of the tumour. It is often difficult to obtain measurements of tumour size with A-scan, thus B-scan USG is usually preferred for tumour biometry.
Three-dimensional Ultrasonography
While performing standard 2D-USG, the operator is required to create a mental 3D representation of the tumour. The captured 2D images do not show tumour volume or surface characteristics. The images may not include the tumour apex in atypically shaped tumours. In contrast, 3D-USG collects echographic data from a large series of 2D-USG images that are quickly acquired and assembled using a computer algorithm. The resulting 3D images can be rotated, sliced or viewed in different planes.7
Tumour biometry using 3D-USG in 42 patients with choroidal melanoma found this technique to be as reproducible as clinical examination and standard USG for measuring tumour diameter and height. 3D-USG was slightly more accurate in its ability to assess tumour volume as it accounts for geometry in a superior manner than standard USG.8 3D-USG has a shorter examination time and does not require additional operator training.7
Colour Doppler Imaging
Based on the Doppler phenomenon, colour Doppler imaging (CDI) is a non-invasive technique used to study blood flow. The Doppler phenomenon states that the frequency of a wave changes when the observer or source move relative to one another. CDI displays colour-encoded flow information in a 2D-USG image and can be used to visualise small blood vessels in the intrinsic circulation of the tumour. Reduction in the number of vascular regions may also serve as an indicator of response to treatment.
In one study of 44 intraocular mass lesions, abnormal Doppler shifts were demonstrated in 39 cases.9 Using CDI, orbital haemangioma and malignant melanoma show significant difference between maximal and minimal blood velocities, resistance to flow and pulsatile index, with haemangiomas having slower flow and lower resistance than melanomas. Also, higher maximal flow in the central retinal artery and posterior ciliary arteries is observed in uveal melanoma (see Figure 4).10
Ultrasound Biomicroscopy
High-frequency UBM allows for imaging of living structures at microscopic resolution. UBM uses ultrasound in the range of 20–100 MHz to obtain resolution at the level of 25 μm.11 UBM can be used to examine any part of the eye that can be approached directly from the surface, usually the cornea and anterior segment structures (including the iris and ciliary body). The conjunctiva, underlying sclera and peripheral retina can also be examined if the eye is rotated away from the region of interest. Examination of the posterior pole, however, is not possible at this time with standard UBM techniques.
With regard to uveal melanoma, UBM is primarily used for localising and measuring iris and ciliary body lesions. The technique is particularly useful for determining the degree of posterior tumour extension and distinguishing solid from cystic lesions (see Figure 5). Serial measurements allow monitoring of growth and spread of the tumour. UBM characteristics have been shown to have a high correlation with histopathological features.12 The shape and local extension visualised by UBM have been shown to be similar to those observed by histopathology. The internal reflectivity seen on UBM has also been shown to correspond with the features found histologically; for example, tightly packed tumour cells have shown low reflectivity whereas loose cellular structures have demonstrated higher reflectivity. One of the major advantages of UBM is its ability to distinguish a localised iris lesion from a ciliary body tumour involving the iris, both of which can appear similar on clinical examination. Small ciliary body tumours undetectable by conventional USG can be easily detected; internal detail can be discerned and allows for precise demarcation of posterior margins needed to plan surgical excision.11 UBM offers superior visualisation of the posterior margin and characterisation of tumour configuration in comparison to anterior segment OCT (AS-OCT).13
Angiography
Fluorescein Angiography
The retinal vasculature can be observed with fluorescein angiography; however, this form of angiography is rarely part of the standard spectrum of tests used in the diagnosis of choroidal melanoma. Small melanomas may show normal fluorescence or hypofluorescence because of blockage of background fluorescence. Larger tumours usually reveal patch-like hypofluorescence or hyperfluorescence.4 They may also show hot spots caused by RPE leaks, which in the late phase, typically show leakage. In some cases of choroidal melanoma, intrinsic tumour circulation (‘double circulation’) may be visible.
Indocyanine-green Angiography
Compared to fluorescein angiography, indocyanine green has a peak absorption in the infrared spectrum, enabling it to penetrate the retinal layers and visualise the deeper choroidal circulation in a superior manner.14 As a result, ICG is useful for visualising tumour vascularity (see Figure 6). In amelanotic melanomas, there is earlier onset of fluorescence (less than one minute) compared with pigmented melanomas (three minutes). The fluorescence itself can vary and can be hypo-, iso- or hyperfluorescent depending on pigmentation of the melanoma. ICG can also help to distinguish choroidal melanoma from other tumours such as choroidal haemangiomas or choroidal metastases. Choroidal haemangiomas have an early onset of fluorescence, early maximal fluorescence (within five minutes) and a ‘washout’ effect in the late phase, whereas choroidal metastases reveal diffuse fluorescence with isofluorescence in the late phase. Confocal ICG may also help to predict risk of growth in a choroidal nevus by observing complex microvascular patterns.15,16
Optical Coherence Tomography
Anterior Segment Optical Coherence Tomography
Using light at 1310 μm with a rapid scanning technology, AS-OCT can image the anterior segment and is capable of obtaining a resolution of 17 μm with tissue penetration of 3–4 mm,17 whereas ultrasound biomicroscopy has a lower resolution of 25 μm but higher penetration of 5–6 mm. As a result, AS-OCT is a useful tool for evaluating superficial lesions, particularly tumours anterior to the iris pigment epithelium (see Figure 7). For larger lesions, or those arising in the iris pigment epithelium, shadowing occurs and posterior margin visibility is poor compared with ultrasound biomicroscopy.13 For these reasons, AS-OCT has limited use in the evaluation of uveal tumours.
Spectral Domain Optical Coherence Tomography
Due to the fact that the choroid cannot be visualised using spectral domain OCT (SD-OCT), it is not helpful in the diagnosis of choroidal melanoma. However, SD-OCT can be used to document the retinal and RPE changes associated with choroidal melanoma or high-risk choroidal nevi (e.g. those with associated sub-retinal fluid) (see Figure 8). OCT may serve to differentiate a choroidal melanoma from a melanocytoma, which demonstrates a superficial retinal component in melanocytoma.
Using 3D SD-OCT it was observed that, compared with choroidal nevi, choroidal melanomas more commonly presented with sub-retinal deposits, sub-retinal fluid and intraretinal edema.18 However, visualisation is limited to the anterior aspect of the tumour with currently available OCT systems.
Enhanced Depth Imaging
Standard SD-OCT is unable to visualise the choroid and outer layers of the eye such as the sclera. Attempts to decrease scatter and absorption by the RPE, using 1050 nm light instead of the standard 800 nm light, unfortunately resulted in low scanning speeds and movement artefact and a deteriorated image quality. Recently, enhanced depth imaging (EDI), a new method of obtaining images of the layers beyond the RPE, has been developed. EDI is made possible by bringing the OCT scanner very close to the eye to obtain an inverted image.19 EDI SD-OCT allows visualisation of the choroid and is useful for further characterising choroidal tumours.
EDI SD-OCT can assess choroidal tumours qualitatively (tumour outline, reflectivity, shadowing, inner sclera visibility) and quantitatively (diameter, thickness) (see Figure 9).20 Choroidal melanoma has a band of high reflectivity in the choroid and demonstrates posterior shadowing. SD-OCT can also assess and accurately measure small tumours that are undetectable by USG.
Metastatic Uveal Melanoma
While the use of imaging techniques for the diagnosis and documentation of primary uveal melanoma is fairly standardised, there is lack of consensus on protocols for screening for asymptomatic metastatic uveal melanoma.
The liver is the most common site of metastases from uveal melanoma. Once liver metastases occur, the median survival time is approximately six months. Earlier detection of metastases, when small and localised, may enable the use of newer life-prolonging treatments or increase the effectiveness of presently available treatments. Screening tests commonly used, such as hepatic USG, chest radiography and liver function testing, have high specificity but low sensitivity. Whole body PET-CT has gained some acceptance as a screening tool at initial diagnosis; it is possible that early intervention for small, localised metastases could offset the higher costs associated with this method of screening.21
A survey22 evaluated practice patterns among Collaborative Ocular Melanoma Study (COMS) centres for the diagnosis of metastatic spread from uveal melanoma at diagnosis and follow-up and found that, at presentation, 17 % of North American COMS specialists versus 95 % of European centres performed one hepatic-imaging study (USG, CT, MRI or PET). This gap widened at follow-up when only 3 % of specialists in North America compared with 79 % in Europe performed hepatic imaging; 70 % preferred USG every six months and 18 % every year. American specialists usually obtained chest X-rays and liver function tests as recommended by COMS.23
It has been suggested that liver function tests on a biannual basis combined with hepatic USG would detect up to 98 % of liver metastases.24 The authors follow this recommendation in the management of their patients.
There is keen interest in identification of blood biomarkers for convenient identification of metastasis, treatment monitoring, treatment selection and possible risk stratification for adjuvant therapy. Levels of vascular endothelial growth factor (VEGF) in the serum can be measured when microscopic metastases are present and they parallel tumour burden. However, VEGF lacks specificity and research to identify other VEGF subtypes or receptors may increase its utility.
Levels of circulating tumour cells and levels of tyrosinase or MelanA/MART1 transcripts by reverse transcription polymerase chain reaction can be used as a risk factor for development of metastases.25,26 Melanoma inhibitory activity,27,28 osteopontin,29 S100 beta,29,30 hepatocyte growth factor, epidermal growth factor and insulin-like growth factor have been associated with metastatic uveal melanoma and may be useful as a screening test in the future.31 ■